Join the 4 percent! There’s help for vaginal dryness
Join the 4 percent! There’s help for vaginal dryness.
During my recent webinar on vaginal and urinary health, I encouraged women who avoid sex because vaginal dryness makes it uncomfortable and painful to share this fact with their partners.
I asked them to put themselves in their partner’s shoes: “How would you feel if your partner doesn’t want intimacy and sex anymore? What would you think? That your partner is no longer attracted by you? Doesn’t love you anymore? Has a lover? That you don’t turn him/her on? You’re no longer sexy?”…
The next day I received an email from a woman who attended the webinar, thanking me for suggesting she explain to her partner why she’s been avoiding sex. She said that after the webinar “I shared with him about my discomfort and dryness issues and told him that I do love him and that I am not having an affair. I think he was really relieved. Good advice”!
It may be difficult to start this conversation and to explain what you are experiencing, so here are some tips to “Talking with your partner”.
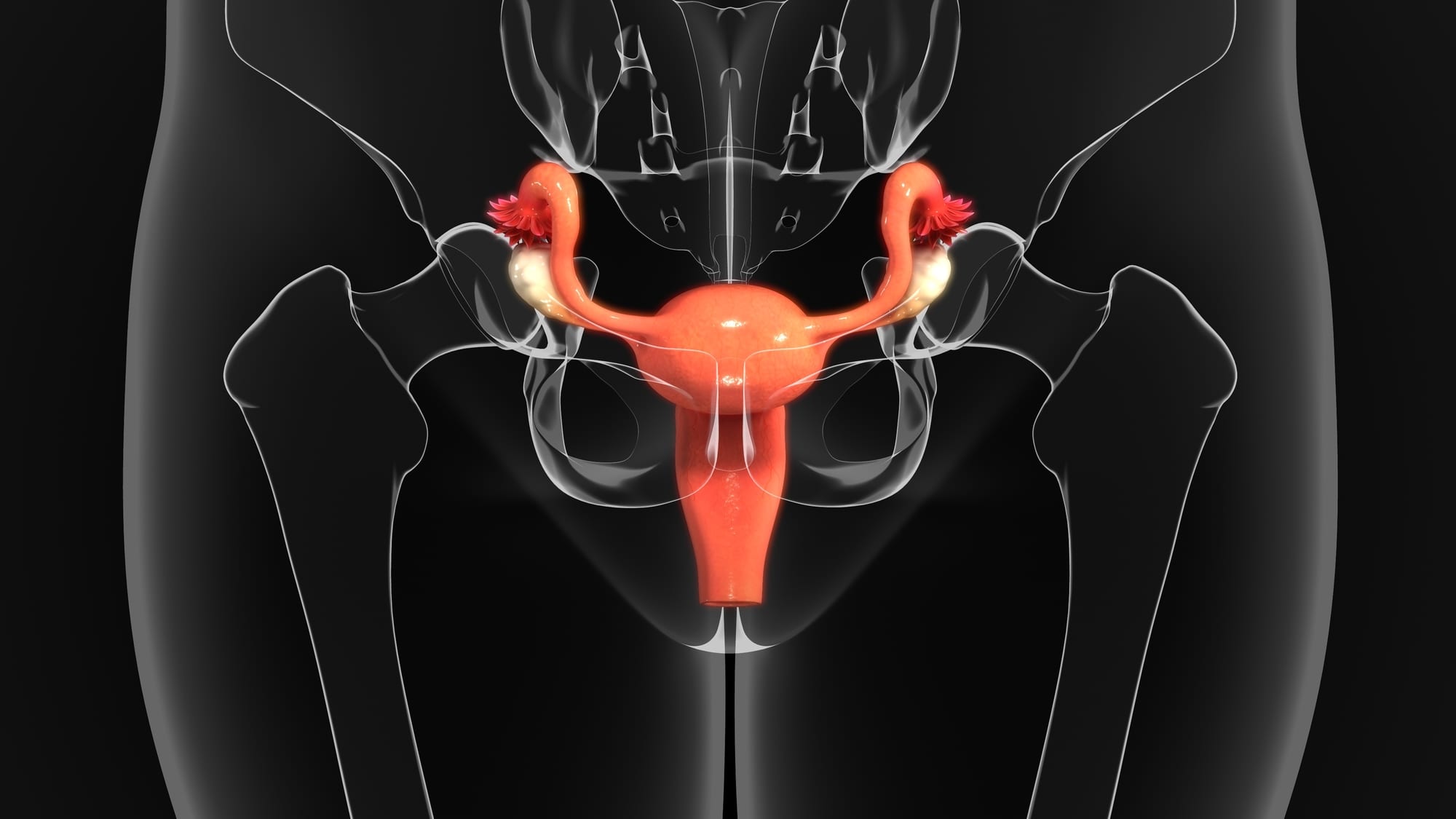
Vaginal dryness is more likely to happen when estrogen levels are low. This can happen due to natural menopause (including during perimenopause), and due to induced menopause such as surgery to remove the ovaries and certain cancer treatments that affect the ovaries. Vaginal dryness can also occur while breastfeeding, during periods of stress, when using certain medications for the treatment of fibroids or endometriosis, and when taking antidepressants and some cold and allergy medications.
You may notice lack of lubrication, decreased arousal, and difficulty achieving orgasm. Penetration may cause pain because the vaginal opening has become narrower, the lining of the vagina is thinner and less elastic, and the vulva and clitoris may even shrink without estrogen. This cluster of symptoms is called vulvovaginal atrophy (VVA).
Around 50% of women are bothered by these symptoms but only 4% receive treatment. Why do you think that happens?
Several reasons come to mind:
- Women assume this is part of aging and there’s nothing they can do about it; it’s just something they must put up with
- Women don’t know help is available
- Women don’t know where to go for help
- Women don’t know what to buy to alleviate their symptoms
- Women suffer in silence and don’t complain to their doctors about their symptoms
Vaginal discomfort affects a woman’s sexuality and self-esteem, upsets the relationship with her partner, and decreases intimacy, sexual desire, and quality of life.
It’s not only sexually-active women who are bothered by vaginal and vulvar changes due to decreased estrogen. Many women feel uncomfortable riding a bike, sitting for prolonged periods, or wearing tight clothes.
Don’t be one of the 96% of women who receive no help for their vaginal symptoms. Join the 4 percent!
There are many therapies to help VVA symptoms:
Regular sexual stimulation
This increases blood flow and lubrication. Remember, if you don’t use it, you lose it!
Over-the-counter products
- Vaginal lubricants (non-hormonal) can be used during intercourse to add lubrication, reduce friction, and improve pleasure. They can be water-based, silicone-based, mineral oil-based, or plant oil-based.
- Vaginal moisturizers (non-hormonal) are designed to adhere to the vaginal mucosa, allowing cells to retain moisture. They are applied regularly to the vagina and vulva, and are longer-acting than lubricants. An example is Repagyn, an ovule containing hyaluronic acid, a substance that provides moisture and a soothing effect. This product is behind-the-counter meaning you must ask the pharmacist for it.
Do not use products that have added flavours, a warming sensation, or are scented, because these can cause irritation. As with many things in life, but especially with products you use on your vulva and in your vagina, less is better.
Pelvic floor therapy
Sometimes the pain is caused by very tight pelvic muscles rather than by thin and dry vaginal tissues. A physiotherapist specializing in pelvic floor therapy (PT) may be very helpful. Even during COVID you can book a FREE Virtual Discovery Pelvic Health appointment.
Low-dose vaginal estrogen
Lubricants and moisturizers may not be helpful, or they may stop being helpful, because they add lubrication and moisture to the area but do not treat the thinning of the vaginal tissues which tends to worsen over time. The most effective treatment for VVA is local estrogen, which is available on prescription as a cream or a vaginal ovule.
If low-dose estrogen vaginal therapy is recommended for you, do not be put off by the warnings and precautions on the accompanying product insert. Due to their low dose, the systemic (affecting the whole body) absorption of the estrogen is very low, much less than if you were taking an oral pill, for example, and the adverse effects are less likely too. But, for many reasons, the information in these low-dose vaginal products doesn’t reflect that difference and instead lists the same warnings and precautions as for the oral products. It doesn’t make sense. I, and many other experts, believe these warnings do not reflect the best scientific knowledge. Many groups advocating for women’s health are trying to get the FDA and the manufacturers to change the information in these pamphlets.
Prasterone
This is a non-hormonal vaginal ovule therapy, and a new therapy in Canada.
Ospemifene
This is a a non-hormonal oral tablet expected to be available in Canada sometime in 2020.
Laser
This treatment is done in the doctor’s office and is fairly expensive.
Which therapy should you choose?
Usually, unless VVA is severe, lubricants and moisturizers should be used first.
If these products do not help—or they stop helping—then your next therapy options should be based on the severity of symptoms, contraindications for therapy, medical conditions, medical history, and your personal preferences. A ten-minute physician’s visit usually isn’t enough to go over everything that needs to be addressed.
Women’s self-esteem, quality of life, and relationships suffer when vaginal dryness and painful sex aren’t addressed. Stop suffering alone and in silence. Join the 4 percent! There’s help. I can help you!
Teresa Isabel Dias is a pharmacist and Certified Menopause Practitioner (NCMP) who provides education and support on symptom management for women at work and at home so they’ll feel like themselves again and enjoy a vibrant and productive life.
Grab a quick guide and subscribe to the MenopausED Newsletter on the MenopausED home page.
If would like to know how Teresa can improve your menopause transition then schedule a complimentary Discovery Call at MenopausED.org.